62 YEAR OLD FEMALE WITH LOOSE STOOLS AND VOMITINGS.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
62 year old female farmer by occupation came with chief complaints of
-Loose stools since 2 days
-Vomitings 2 days ago
History of present illness:
-Patient was apparently asymptomatic 2 months ago when she had a history of fall from her bed then developed pain in her right shoulder .she then approached local doctor for which she was given pain killers but not relieved. She then went to the private hospital and was treated symptomatically by medication.
-2 days ago patient experienced Vomitings 3 to 4 episodes Non projectile, non bilious ,non blood tinged food as Content.
On the same day she had 5 to 6 episodes of loose stools yellow colored, watery non foul-smelling they went to RMP doctor and was treated Vomitings got subsided.
-She then went for government hospital where they started on symptomatic treatment and fluids but was not relieved.
-Since today morning she had 10 episodes of
loose stools
loose stools
-No history of fever,abdominal pain,intake of outside food.
Daily routine:
She is a farmer by occupation used to work in paddy fields but after her history of fall she stopped working.
She wakes up around 5 am early in the morning
Does some household works then drinks tea at 7 am .she cooks food for her family then takes her breakfast at around 10 pm.She takes her afternoon lunch at around 2 pm sleeps for sometime and then helps in household works and completes her dinner by 9 pm goes to bed by 10 pm.
Since 2 days her daily routine got disturbed and she was mostly on liquid diet since 2 days.
Past history:
Not a k/c/o Hypertension ,DM, TB,Bronchial Asthma, Epilepsy, CVA and thyroid disorders.
PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative
Moderately built and moderately nourished
Well oriented to time place and person
VITALS
TEMPERATURE:Afebrile
Pulse rate: 89bpm
BP: 130/90 mmhg
No Pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION:
Shape of abdomen: Distended
No tenderness
No palpable mass
Dull on Percussion
CNS EXAMINATION
No focal neurological deficit
CVS EXAMINATION:
Cardiac sounds S1 S2 heard
No murmers heard.
RESPIRATORY SYSTEM
Bilateral air entry present
Normal vesicular breath sounds heard
Trachea: central
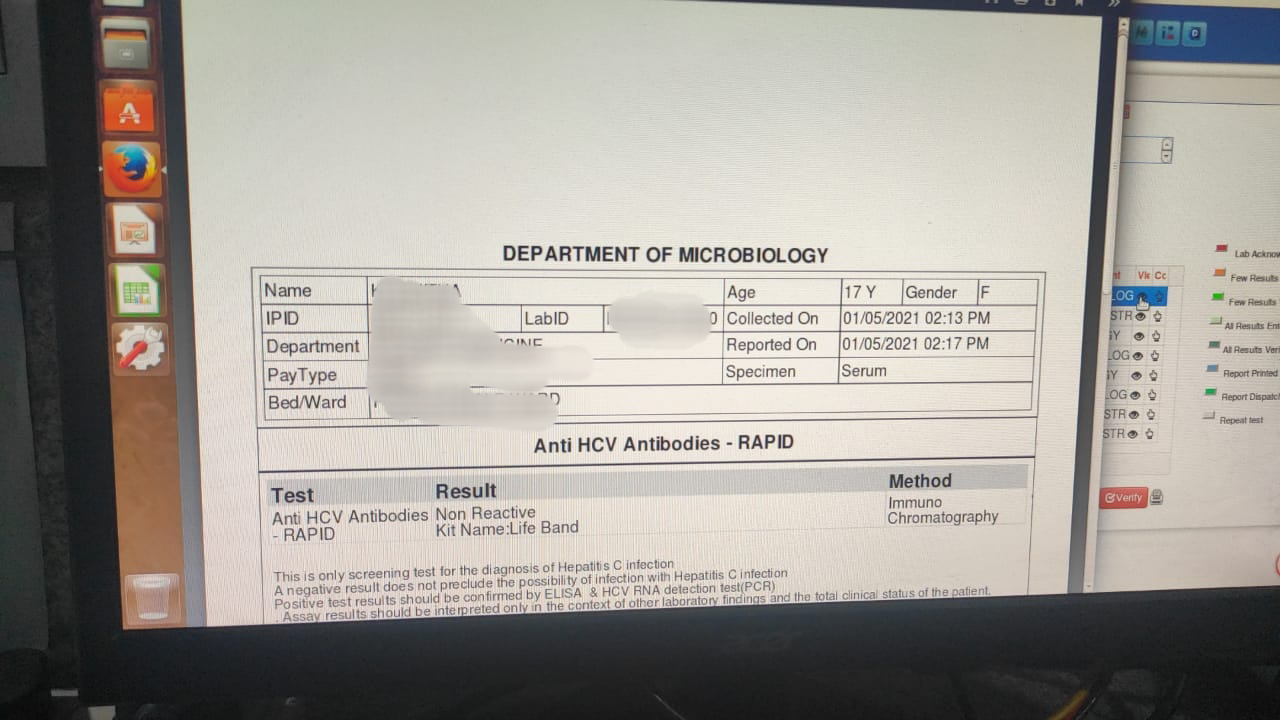
Clinical images:
RBS:
RFT:
Acute gastroenteritis
TREATMENT:
1.Inj Metrogyl 500 ng iv/Tid
2.Iv fluids NS @75 ml per hour
3.Inj Pan 40mg iv/od
4.Tab sporolac Ds po /TID
5.Tab Redotil 100 mg Po/BD
4.2 ORS in 1 liter of water 200 ml after every episode












Comments
Post a Comment