60 YEAR OLD FEMALE WITH FEVER, VOMITINGS AND ABDOMINAL PAIN.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Chief complaints:
60 year old female came with chief complaints of
-Fever since 1 month (on and off)
- Vomitings since 5 days
-Abdominal pain since 5 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic
2 years back then she developed Bilateral knee pain and back pain insidious in onset gradually progressive and was relieved by medication.
6 months ago patient developed pain in the left side of chest region non radiating type not a/w any palpitations sweating and shortness of breath. No aggrevating or relieving factors for which she was hospitalized and treated.
[According to patient attendar patient had a history of trauma to the left side of chest at the age of 30 years for which she used to experience pain on and off ]
3 months ago patient developed Loss of appetite and
generalised body pains for which she used to go to nearby local hospital for treatment. Relieved by taking medication.
1 month ago patient developed fever low grade type intermittent in nature relieved by medication.
-Patient complains of vomitings since 5 days 4 to 5 episodes occurs after every meal food as Content nonprojectile non bilious non blood tinged.Aggrevated by taking food.
-Diffuse abdominal pain since 5 days No aggrevating and relieving factors.
-Patient also complains of Chest pain since 5 days burning type insidious radiating to back.
-Patient also complains of Shortness of breath grade 2 MMRC relieved by taking rest.
PAST HISTORY:
Patient had a history of trauma to the left side of the chest region .
Not a K/c/o Hypertension, DM, TB, Bronchial Asthma,Epilepsy and thyroid disorders.
Daily routine :
Patient used to knit wooden items for living and used to experience shortness of breath while working used to take small breaks for relief between the work.She stopped working since 2 years and stays at her son's home while her daily routine includes waking early in the morning around 6 am and drinks tea at around 7 pm and does some household works and takes her breakfast at around 9 pm mostly rice.She does her lunch at at around 2 pm and takes nap for 1 hour.
She takes her dinner at around 9 pm and sleeps by 10 pm.
Her daily routine got disturbed since 3months as she is experiencing loss of Appetite.
Her Sleep got disturbed by pain.
Personal History:
She takes Mixed diet
Bladder movements regular
Bowel movements reduced
No Addictions
Family history:Not significant
PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative
Thin built and moderately nourished
Well oriented to time place and person
VITALS
TEMPERATURE:Afebrile
Pulse rate: 86bpm
BP: 110/70 mmhg
No Pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
SYSTEMIC EXAMINATION:
ABDOMEN EXAMINATION:
Shape of abdomen: scaphoid
No tenderness
No palpable mass
CNS EXAMINATION
No focal neurological deficit
CVS EXAMINATION:
Cardiac sounds S1 S2 heard
No murmers heard.
RESPIRATORY SYSTEM
Bilateral air entry present
Normal vesicular breath sounds heard
Trachea: central
Clinical images

Chest xray PA view
Widal test:
Dengue NS1 antigen:
ESR:
Hemogram:
Reticulocyte count:
Serum iron:
FBS:
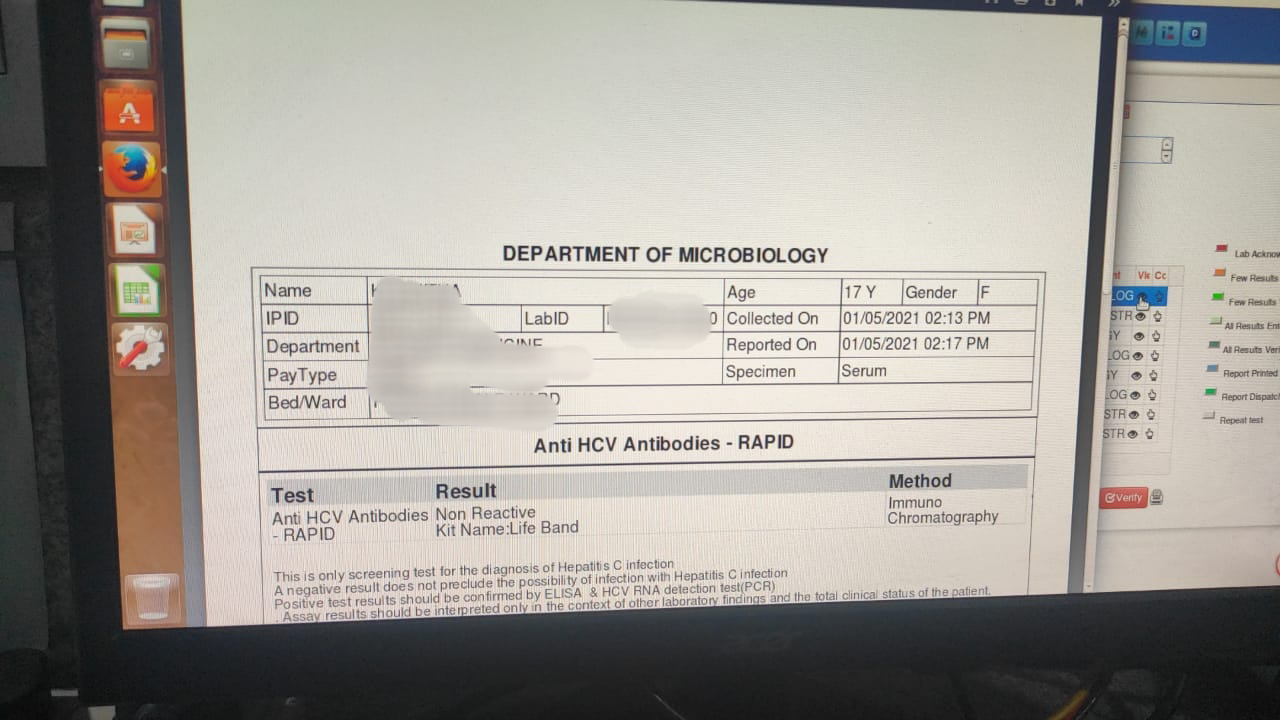
HCV:
SERUM CREATININE
SERUM ELECTROLYTES
LFT
HIV:
HBSAG:
CUE

2DECHO

Usg abdomen
Provisional diagnosis:
Oral and esophageal candidiasis
Anemia due to chronic disease
Treatment:
1.Tab.Zofer 4 mg po/sos
2.Tab.Pan 40mg Po/OD
3.Tab.Fluconazole 150 mg OD
4. Tab.Bcomplex OD
5.zytee gel for local application 15 min before taking food
6. Candid Oral paint for local application 3 times/day
7. 2%Betadine gargles 3 to 4 times a day




















Comments
Post a Comment